
Acute injuries are sudden and brutal. When my accident happened, I lost my independence in an instant. It was a traumatic incident that resulted in a cascade of negative effects on not just my physical, but mental health.
The Emotional Journey From an Acute Traumatic Injury Through Recovery
It was a regular November morning. A snow storm had passed through the night before. I put on snow gear and was headed out into the city–cheerful and excited for the day, lost in thought.
Suddenly, I tumbled down a stairwell in the subway and landed sitting up with my right ankle broken in three places.
As I sat on the stairwell, buzzing New Yorkers walked over me, yelling to “move out of the way” and “just get up.” No one helped. I begged an MTA officer to call an ambulance. He rolled his eyes. It was not obvious how injured I was because I was bundled up and sitting on my foot.
The ambulance transferred me to a nearby ER. I sat in a hospital bed and was wheeled from room to room, without knowing where I was going or what was happening. No one would speak to me until the doctor arrived. They wouldn’t even make eye contact.
Nurses were touching my pelvis and spine to ensure the injury was confined to my ankle, but I was being treated as if I was unconscious. Finally, a doctor explained I had a trimalleolar fracture, and attempted to manually adjust my bones back into place–twice. I went from low whimpering to animalistic, uncontrolled screaming.
Despite being given a combination of narcotics and local anesthesia, I was in no way numb.
When I was transferred from the ER to the hospital for surgery, I was put on standby. My injury wasn’t critical from a safety/survival standpoint, and I was generally healthy, so I waited three days for surgery. Each day I was starved and delirious. My cousin and mother stood in as caregivers and advocates to get me into surgery.
The Emotional Impact of Feeling No Control
When it was time for surgery I was wheeled into the operating room by residents I had never met. “Do you speak English?” Asked a nurse. I replied “yes,” frightened that no one knew who I was or what I was doing there.
The surgeon introduced himself and went through the procedure instructions expediently. He then pulled a Sharpie out of his pocket, wrote his name on my injured leg and said: “you’re mine now.” I think he was trying to be comforting, but I was terrified. They whisked me to anesthesia and I was knocked out.
The surgery was successful. But as a result, I had no control over my body (from the physical impairment) or my mind (from heavy narcotics).
The hospital room was full of people monitoring me–touching my arms to get vitals, sponge baths, administering pain meds. I tried negotiating my circumstances where possible. For my dignity, I did not want to use bedpans. Instead, I worked to use a walker to go to the bathroom.
I wanted to leave the hospital so badly. I remember refusing meds during an acute pain attack in an effort to be discharged and the nurse said to me, “You are suffering. I promise you will leave the hospital soon, but stop suffering.”
The Challenge of Processing Intense Medical Experiences
Trauma comes in waves. I suddenly remember tender moments… like when my cousin and a nurse washed my hair in the sink since I wasn’t allowed to get wet. Or the way the surgeon knowingly looked into my eyes when I told him I need full range of motion in my foot. Or the resident who was comically too casual given the gravity of my situation. Or the smile on the faces of the hospital staff when I requested only chocolate ice cream for dinner… and the way my mom spoon-fed me said ice cream.
I also remember the week I spent waking from the same nightmare holding my ankle as I did after the fall–re-enacting my accident and jerking my leg in my cast.
Reclaiming Empowerment Through Getting Off Narcotics
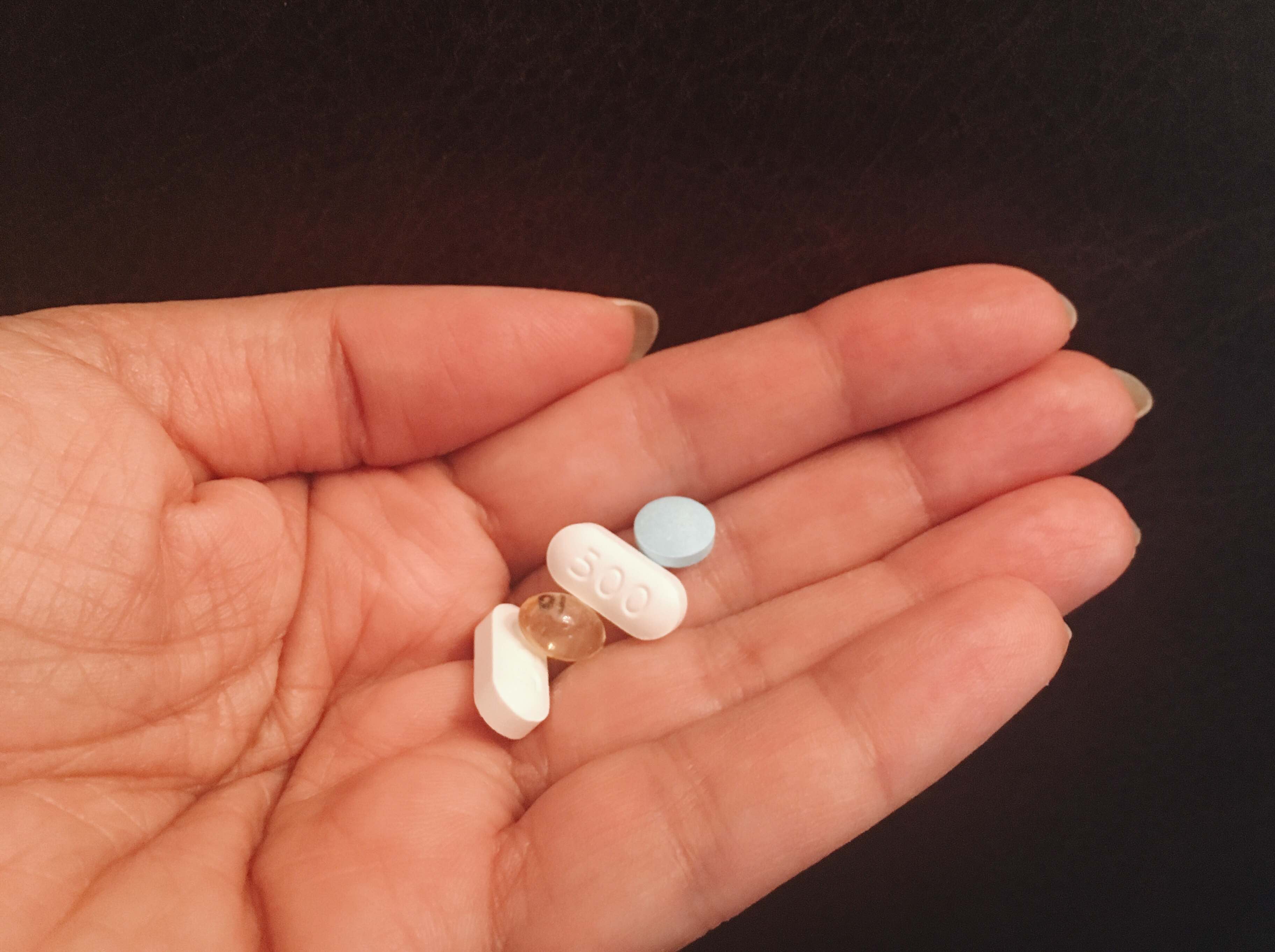
I was given a full bottle of OxyContin and Tylenol for pain at home. After being on narcotics for more than a week in the hospital, returning to the familiar environment of my apartment, I started to notice the effects. I had weird in-between dreams where I couldn’t tell the difference between waking and sleeping life.
I was told that I should wean myself from the meds, but not given to instruction how.
My plan was to stop narcotics completely during the day, and take meds in the evening as needed. That first morning, after about six hours off of drugs, I started to feel my foot. It had previously been numb to any sensation.
Now my foot was waking up. I felt gurgling, tingling, pinching. Going from no sensation to sensation is intense. Coupled with generalized fear, I was terrified of the possibility of pain. I screamed to my mom to bring the narcotics and she ran to me.
My mom was all too familiar with my screams of pain from the hospital. She said to me “what do you feel?” That skillful question took me out of the black and white “pain” or “no pain” and into the exploration of sensation.
I ultimately determined that I was feeling sensation, and while the sensation was not pleasant, it didn’t warrant a pain-killer. I managed to get off narcotics within two days.
Had my mom not slowed down my reaction to the sensation, I’m not sure I could have done what I did. That was my first moment of reclaiming discernment and choice in my recovery.
Re-Establishing Boundaries to Help Restore Mental Health
In the hospital, there was no part of my body that felt like mine. In my apartment, I had to fight to retrieve every piece of physical independence while being realistic about my own abilities.
Not being allowed to shower alone (shower stalls are too slippery), left me literally naked in front of friends I had never exposed myself to. I broke down over small things like not being able to get my foot into my boot or being unable to get ahold of my doctor.
People I was not intimate with were seeing my physical and emotional vulnerability in a way that left me raw.
However, as I softened into my new reality, I realized that despite the loss of control (and sometimes dignity), I did have choices. I had the choice to embrace the love and the care that all the individuals who came into my home gave me. With that choice came a power; a feeling of love and of non-reciprocated care.
Over time, the physical empowerment came back as well. I was able to shower alone, prepare food on my own, and go back to a normal life over the course of months.
Tracking Recovery Progress to Reclaim Independence
A big part of regaining independence after this acute traumatic injury was my ability to assess where I actually was and to test my own limits. Tracking my progress each day was important.
It was a big deal to carry tea with a steady hand from the kitchen to my living room. Previously my hobble was too precarious to have hot liquids in my hand. The ability to walk up and down stairs without a crutch was progress. The day I was able to shower standing up was a highlight.
Celebrating small miracles was important, and kept me on track. I saw tangible differences in my resilience, in my mood, my outlook, and my priorities. The last thing to come back was learning to trust my own body again.
Self-Massage to Regain Feeling and Return to the Body
The story of my accident is my own, but anyone who has suffered a life-altering injury can relate to the trauma of sudden change and the bravery it takes to advocate for yourself. It is exhausting, empowering, and life-changing.
It is easy to disassociate while pushing through the pain of simple things, like walking. It took me time to even consider trusting my body again–I was terrified to feel.
I started the process of feeling again by using the Roll Model® Method therapy balls after a couple of months of healing. I moved very slowly and listened to what my body needed.
Below is a gentle massage for the ankle I practiced. Note that the scar was well healed and I was cleared by a physician and a physical therapist first.
The gentle pressure from the therapy balls helps to desensitize the ankle to stimuli, which is vital after a traumatic event since the nervous system is on high alert in the injured area. However, it’s important to note that the pace (and the depth) of pressing into the therapy balls is entirely your choice.
You get to modulate your self-massage, which can help you reclaim a sense of autonomy and control over your physical self.
Gentle Ankle Massage with Therapy Ball
Props: Yoga Tune Up® Therapy balls, classic set
Sitting on the ground, bend your right knee.
- Place one therapy ball to the outside of the ankle, and move the right knee down toward the ground, pinning the ball between the outside of the ankle and the ground.
- Plow the ball from the outside of the ankle to your Achilles’ tendon, letting the therapy ball tug at the skin gently.
- The pressure is to your tolerance.
- Keep the ball compressed and point and flex your foot at the ankle joint.
- Move slowly, and do not force this movement. It is not about moving to your end range, but rather gentle, tolerable mobilization.
- Maintain the position and pressure, and use one hand to spin the ball into the tissue.
Repeat steps 1-3, placing the ball to the inside of the ankle
Related Article: Beyond Pain Management: Disrupting The Pathways of Pain
Learn more about our Therapy Ball Products and Programs
Interested in video and blog content targeted to your interests?














Sierra, This was my favorite article on the Tune Up Fitness ® blog! It brought tears to my eyes and echos from my past of a traumatic injury I suffered in my spine that took 18 months of consistent and dedicated rehab. I want to express my gratitude for your your willingness to speak truth in such a raw and vulnerable experience. It is so incredible how the mind and body connection evolves together in a way that gets us through the physical trauma and the mental and emotional challenges that come with it.
I was most touched by the statement you made about learning to trust your own body again. A pure statement of deep truth on the silent partnership we share secretly in the intimacy of our own body. Many of us take that dynamic for granted. It isn’t until we face something traumatic that we see the partnership at play-the hidden silent observer that watches from within as we go about living our life and make choices without even knowing of its presence. It isn’t until we come into a situation by accident that suddenly something within us feels betrayed and untrusting. It is real! I can completely relate to this sentiment of learning to trust your body. Such an important and transformative point that many people refrain from sharing.
Lastly, I just want to say that I felt like I was with you in your journey through accident, surgery and recovery. You’re a powerful communicator and have a talent for communicating empathically. I can imagine how going through all of this was in NYC, as I lived there during my studies at John Jay, and am aware of the stairs, bathtubs and lack of eye contact amongst city goers. Your strength to persevere through trauma, and while living in NYC all the while, makes you a superhero. <3
Amazing and so inspirational! Thanks for sharing your journey ❤️
I can’t imagine going into surgery with all of hostility and impersonal care you received beforehand. I’m glad you had loved ones who could see you through your trauma. Kudos to you and your mother for being able to separate pain and sensation. I think narcotics are too carelessly prescribed. So happy that the yoga therapy balls were able to continue your path of self-care and healing.
Thanks for sharing your story. To recover from an accident like that is not easy. The good news is that you made an excellent use of the therapy balls to heal.
Going through severe injury traumas is horrible, by the time you are at home sometimes being unable to move or coordinate because of the injury your body has this is the most horrible part, but is important to recognize that this is a recovery process, so the way Sierra explains each and every step of her recovery is a very nice thing to do, this can show people that even when times seem harder and in those moments that you might think that you may not go through that and/or survive you can recover from anything.
Thank you Sierra, for again being vulnerable and sharing your experience. Healing takes time, and involves so much more than just repairing the physical scars. Small victories are important, and add up… thank you for allowing us to celebrate yours with you.
Thank you for sharing such a raw, unfiltered account of your experience. It is a true testament to your willingness to sit with the uncomfortable and move through it. You have so much insight to offer because of it.
I just did a trauma-informed yoga workshop and the instructor implemented Yoga Tune Up therapy balls as a way to feel sensations in the body and to downregulate the nervous system. The YTU allows people to feel their sensation and add the pressure that they need.
I can totally relate with this blog as I am too currently dealing with acute injuries and the only thing that has helped me has been acupuncture, the tune up therapy balls, and corrective exercises. These therapy balls really are miracle workers.
This discussion is not to soon!! The common use of narcotics for pain without help to get off of the pain pills is all to common. Its nice to read about other options.
I can relate to this on a professional and personal level. I work with patients after they have injured themselves and their life is turned up side down in some degree. I always encourage and help them see the progress towards their goals. But when it happen to me, both worlds turn upside down. I couldn’t work, learned to feed myself with my other hand, get dress/ shower differently. I too went down a dark whole fast but slowly climbed out. Looking back when facing challenges it is important to address the emotional and mental changes along with the physical.
Roll model technique not only help with the injury but also gives some control back to person to help themselves.
What a powerful story about the holes in the Western medical system, the powerful role our support network plays in our lives (should we be fortunate to have one), and an embodied approach to healing and self-care. It is heartening to see so much more discussion about health, medicine and healing, and ways we can all empower ourselves to get better and, I believe, contribute to bettering existing systems.
There are so many benefits with the Roll Model® Method therapy balls everyone should have!
Impressive to see how the general medicine provides us with the easy solution. Is the medication, in addition, in high doses. It’s like nothing else is possible because it does not pay $$$. Let’s continue to spread the good news that there are other alternaties such as self-massage with balls, breathing, méditation, supervised yoga, and so on….These are our own choices….
What a story. It makes me think how fragile we are and how in seconds we can loose the things that we always take for granted, like independence, walking, etc.. thanks for sharing something so personal, and put out there your vulnerability. ❤️
Self-massage with bullets allows us to becom aware of your body and our feelings. it allows the release of tissues gently. Tune-up balls, just hapiness!
No words can describe the compassion I feel for Sierra.She writes intimately and with brave vulnerability about her ankle injury. The article is a portrait of the activity of doing wellness. She allows to help her and listened to her mother and to her body. She became inquisitive rather than fearful of new sensation. It is beautiful and awe-inspiring to witness.
Thanks for sharing Sierra. Sounds like a difficult experience. You sure do look nice and relaxed in that lead image though and I’m glad the YTU Balls helped!